Robotic Thoracic Surgery Column
Robotic thoracic surgery of total thymectomy
Clinical data
- Medical history. The patient, a 28-year-old woman, was found to be with the drooping left eyelid half a year ago, but did not receive special treatment. A few months later, the symptom gradually worsened and then the patient visited a local hospital. Chest CT showed thymic hyperplasia in the anterior mediastinum. The diagnosis was “thymic hyperplasia accompanied with myasthenia gravis”. She was then orally administered with pyridostigmine bromide 60 mg tid, and the symptoms were controlled. Then, she visited our hospital for further management. The patient’s general condition was acceptable, and there were no symptoms such as chest tightness, shortness of breath, difficulty in breathing or swallowing, or fatigue.
- Physical examination showed slightly drooping left eyelid.
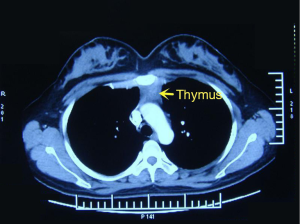
- Auxiliary examination. Chest CT showed a soft-tissue shadow in the anterior upper mediastinum, which had relatively clear margin and homogeneous density (Figure 1).
Pre-operative preparation
Conventional skin preparation was performed. The planned ports were marked on body surface.
Procedures
Anesthesia and body position
After the induction of general anesthesia, the patient was placed in a left lateral decubitus position under double-lumen endotracheal intubation. With his hands put in front of head, he slightly leaned backwards (Figure 2).
Surgical procedures
- Incisions (Figure 3). A 1.2-cm camera port was created in the 6th intercostal space at right posterior axillary line, and two 0.8-cm working ports were separately made in the third intercostal space at middle axillary line and the 6th intercostal space at anterior axillary line.
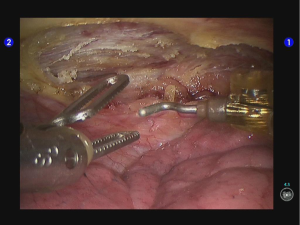
- Inspection of the thoracic cavity with the camera and insertion of the robot arms. The endoscopic airtight trocar was inserted through the camera port to establish 8-mmHg artificial pneumothorax, and then the robotic endoscope was inserted for inspecting any adhesion in the thoracic cavity. Under the endoscopic monitoring, the robot trocars were separately inserted via the two working ports, so as to place the #1 robotic arm (right hand) and the #2 robotic arm (left hand). The #1 robotic arm (right hand) was connected with the unipolar cautery hook, and the #2 robotic arm (left hand) with fenestrated bipolar forceps.
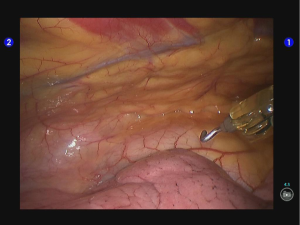
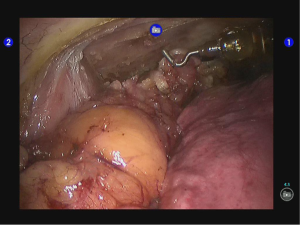
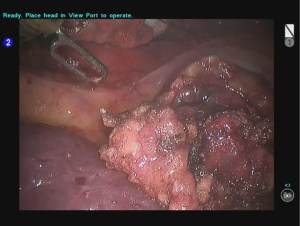
- Inspect the lesion and its relationship with the neighboring tissues/organs. The anterior mediastinum had a full appearance, with a large amount of adipose tissue (Figure 4).
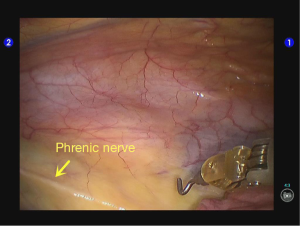
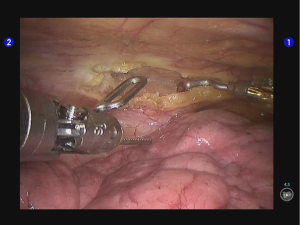
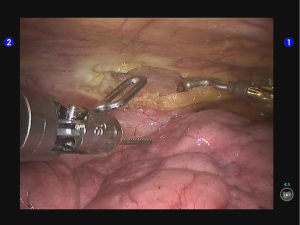
- After the lesion scope was identified, the mediastinal pleura were cut open in front of phrenic nerve (Figures 5-7).
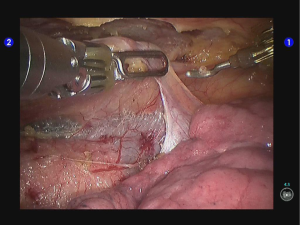
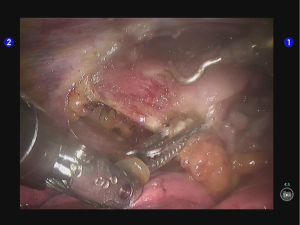
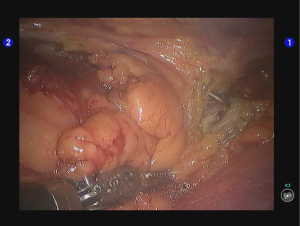
- Beginning from right lower pole of the thymus, dissociate along the pericardial surface upwards till the right upper pole of the thymus, so as to divide the right lobe of thymus (Figures 8-11).
- After the division of the right lobe of thymus, dissociation was performed upwards from the left lower lobe of thymus till the left upper lobe of thymus. Thus, the left lobe of thymus was divided (Figures 12-14).
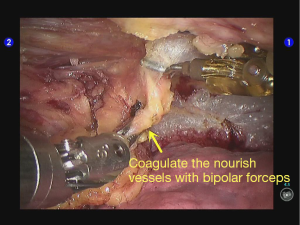
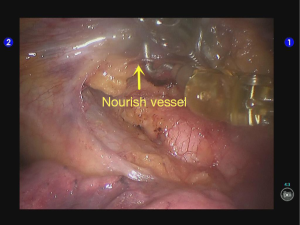
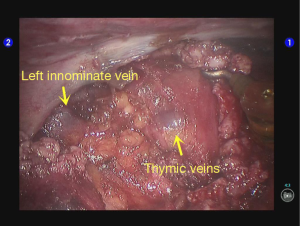
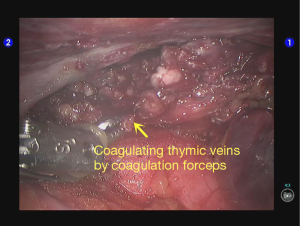
- The upper pole of the thymus is adjacent to the large vessels such as venae anonyma. Therefore, special attention should be paid during the division of the upper pole; in particular, any thermal damage to the vessels as well as vascular rupture/bleeding should be avoided. Two or three thymic veins may enter the lower edge of the venae anonyma (Figure 15). In our current case, the upper part of the lesion was adjacent to the front of the left side of venae anonyma, with the thymic veins clearly visible, which was then sealed with bipolar cautery forceps (Figures 16,17).
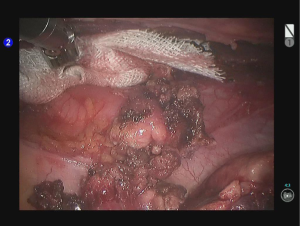
- The whole thymus was removed, and meanwhile the adipose tissues in the anterior upper and anterior lower mediastinum were removed (Figure 18).
- Inspection showed that there was no obvious bleeding or exudate on the wound surface (Figure 19). After the #2 robotic arm (left hand) was withdrawn, the incision was extended to 2 cm. The muscle tissue was divided bluntly. An endoscopic retriever was inserted to harvest the dissected specimen (Figure 20).
- The wound surfaces were sprayed and covered with the sol of Tistat absorbable hemostatic gauze.
- After the robotic arm was withdrawn, any possible incision bleeding was observed under the endoscope. The thoracic drainage tube was indwelled at the camera port before closing the chest.
Postoperative treatment
The endotracheal tube was smoothly removed after the surgery, and then the patient safely returned to her ward. She was orally administered with pyridostigmine bromide 60 mg tid, and its dose was reduced gradually according to her clinical symptoms.
Pathological diagnosis
It was pathologically diagnosed as thymic hyperplasia.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
Cite this article as: Xu S, Liu X, Li B, Ding R, Wang T, Wang S. Robotic thoracic surgery of total thymectomy. Ann Transl Med 2015;3(11):156. doi: 10.3978/j.issn.2305-5839.2015.03.10