Professor Yin Li: “non-tube no fasting”—an innovative management of fast-track surgery in patients with esophageal cancer
Professor Yin Li (Figure 1), Vice President of Henan Cancer Hospital, the Affiliated Cancer Hospital of Zhengzhou University in China, as well as the director of the Department of Thoracic Surgery, is an expert on surgical treatment of thoracic cancers such as lung cancer, esophageal cancer, cardia cancer and thymic carcinoma and so forth.
Prof. Li holds numerous academic tittles in China. Internationally, he is also a member of the International Association for the Study of Lung Cancer (IASLC), the International Thymic Malignancy Interest Group (ITMIG) and the European Society of Thoracic Surgeons (ESTS). He is also the editorial board member of many peer-reviewed journals such as Thoracic Cancer and Innovation (Chinese version), to name few.
With all Prof. Li and his team have achieved so far, the biggest accomplishment that makes him known to all is Fast Track Surgery (FTS) in patients with esophageal cancer, especially the innovative application of “non-tube no fasting” theory. The core of this innovation is to use no nasogastric intubation and encourage early oral feeding postoperatively (at postoperative day 1) in patients following thoracolaparoscopic esophagectomy. This management is proven to be feasible and safe clinically. To gather more scientific evidence, a phrase III clinical trial directed by Prof. Li is underway, with an interim analysis published as poster presentation during American Association for Thoracic Surgery (AATS) 2015.
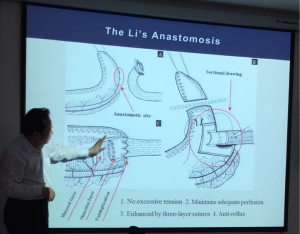
In addition, the Li’s Anastomosis, a creative surgical method developed by Prof. Yin Li based on many traditional ways against anastomotic leak, tremendously improves the surgical outcome and plays a crucial role in FTS for esophageal cancer patients.
In April 22, 2015, I was honored to meet Prof. Li in his hospital and had an interview with him to share with our readers his clinical experience and expertise, as well as the stories behind.
Patients come first—a surgeon’s influence and passion
Esophageal cancer occurs at a high incidence rate in China. The “esophageal cancer belt” from northeast China to the Middle East used to have the highest incidence rate and mortality rate of the disease, and Henan province was, and still is, one of the very regions with the highest incidence.
In February 5, 2015, a middle age male patient was diagnosed with squamous cell carcinoma of the esophagus and hospitalized in Henan Cancer Hospital. A month later, his elder brother, who had been taking care of him, had discomfort and difficulties in swallowing his food and was subsequently diagnosed with the same disease as his younger brother was suffering. These two brothers are both from Henan and underwent surgery performed by Prof. Li and his team. By the day we met them, they were both under recovery with good condition. “They both had food first day after the surgery and they are recovering in a fast way.” Prof. Li told me.
Under the tense relationships between patients and doctors in China, with numerous Chinese doctors complaining about their careers, Prof. Li enjoys the responsibility and happiness of being a surgeon. “A doctor deals with lives, which empowers him with great influence on patients, and for me with great joy as well. Because saving life is something that could not be compared. The hard works of being a doctor is well-known, but the happiness is barely understood.” Prof. Li said.
FTS in patients with esophageal cancer—inspiration and achievement
When being asked about what was the inspiration of applying FTS in patients with esophageal cancer, Prof. Li traced back to the date when he was attending a general surgery meeting held in Nanjing in 2007. “I was at the conference room where Prof. Jieshou Li from Nanjing General Hospital of Nanjing Military Command was giving a speech. He mentioned the use of FTS in gastric cancer and colorectal cancer, and the patients were given food the first day after surgery. I was astonished. Before the closing of the meeting, I rushed back to do some searches on PubMed and found out that there was just one paper related to FTS for esophageal cancer. I carefully read through the paper and it turned out the paper was not really about FTS. At that moment, I realized that there was a ‘new continent’ that had never being explored before. If FTS could be used in patients with gastric cancer, why not esophageal cancer?” Prof Li recounted. At that time, Prof. Li was confident that FTS to be used in esophageal cancer would be successful. And time proves that he was right.
Starting from February 2014, Prof. Li and his team have initiated a prospective randomized clinical trial (NCT01998230): early oral feeding following thoracolaparoscopic oesophagectomy in patients with esophageal cancer, as to explore the efficacy and safety of the “non-tube no fasting” management, compared with the traditional methods. In April 29, 2015, the interim analysis of the trial was published as poster presentation in AATS annual meeting. With 148 patients with esophageal cancer enrolled, 72 patients were randomly assigned into the early oral feeding group (oral feeding at first day after surgery), 76 patients were in the delayed oral feeding group. The results show no significant difference between the two groups in the baseline data, postoperative complications and the incidence rate of anastomotic leakage. While the bowel function recovery time and the length of postoperative hospital stay are significantly shorter in the early oral feeding group than the delayed oral feeding group. Some American surgeons were amazed after the presentation of the poster. While they were just trying not to place the nasogastric tube to reduce postoperative discomfort of the patients, Prof. Li and his team has already been encouraging patients to have food intake orally the day after the surgery.
But things before were not as smoothly as it seems today. Thoracolaparoscopic oesophagectomy, the combination of using thoracoscopy and laparoscopy to resect esophageal cancer, is one of the key factors that largely improved patients’ surgical outcome due to its minimal invasive feature. It is a driving force in the course of developing FTS in esophageal cancer. However, back in 2009, when Prof. Li was just promoted as director of Department of Thoracic Surgery, thoracolaparoscopic oesophagectomy was not as widely recognized and applied. The complicated procedure and technical challenges had scared away many surgeons. While Prof. Li believed that this new surgical technique would bring great advantages to the patients. He insisted in introducing this technique. After several attempts were failed to convince the board of the hospital, he invested his own money to buy the equipment.
Master’s technique—the Li’s Anastomosis
“Prof. Li wishes to improve the clinical technique of FTS every day, even in his dreams when he is sleeping. He is very strict with himself.” One of Prof. Li’s colleagues told me. It is not difficult to see that Prof. Li is a surgeon constantly pursuing for improvements, new technologies and innovations, as long as it does good to patients.
Anastomotic leak, a very severe complication that may occur postoperatively in esophageal cancer patients, is an ever-present “headache” for thoracic surgeons. However, perceived from another aspect, it is also one important key to open the door of better FTS for patients. That’s how the Li’s Anastomosis comes from (Figure 2).
With the advantages of (I) no excessive tension, (II) maintains adequate perfusion, (III) enhanced by three-layer sutures, and (IV) anti-relux, the Li’s Anastomosis is proven to decrease the rate of anastomotic leak and become of key support for the “non-tube no fasting” management.
Prof. Li considers that being a surgeon, it is marvelous enough to focus on one area and become an expert and even a pioneer. It is certain that Prof. Li’s focus will still be FTS in patients with esophageal cancer in the near future. Be it in forms of the “non-tube no fasting” management or “the Li’s Anastomosis”, it all comes to an end for the good of patients—fast recovery, less hospital stay, less cost and higher life quality.
“If there is enough time and energy, I would be happy to do more—to build up a whole system of managing esophageal cancer, from prevention, diagnosis, treatment to multi-disciplined management and precise treatment”, Prof. Li said, “There is a lot to do for patients”.
Acknowledgements
Disclosure: The author declares no conflict of interest.
(Senior Editor: Eunice X. Xu, ATM, editor@atmjournal.org)