Double primary non-small cell lung cancer with synchronous small cell lung cancer N2 nodes: a case report
Introduction
Synchronous multiple primary lung cancer (SMPLC) is a rare entity with an incidence of 1.5-2% per patient per year (1). The first diagnostic criteria for patients with SMPLC were established by Martini et al. in 1975 (2), and were refined by Antakli et al. in 1995 (3). However, not all patients with SMPLC match the above criteria (2). Involvement of the mediastinum is, surprisingly, excluded from these reports, leaving a vast gap in the staging and therapeutic strategy of such patients. The rise of modern diagnostic and imaging methods in addition to new curative and histological techniques are generally encouraged, with the hope of providing better survival rates, as reported recently (4-6).
Case presentation
A 68-year-old male patient, with Eastern Cooperative Oncology Group (ECOG) score 0-1, was referred to our clinic for surgical resection of a left upper lobe mass. A CT-guided biopsy of the tumor was performed a few days earlier, which revealed squamous cell carcinoma.
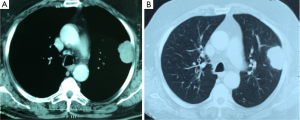
His medical history consisted of heavy smoking (110 PY) and hypertension. Chest-CT with 5 mm-thick images indicated a 4.3 cm diameter mass in the left upper lobe (Figure 1). No pathological lymph nodes of the mediastinum were described, and complete CT scan was negative for distant metastases. Laboratory findings were within normal limits. The spirometry results were quite satisfactory [forced expiratory volume in 1 second (FEV1): 1.78-64%, forced vital capacity (FVC): 2.6-73%].
An open left posterolateral thoracotomy was performed, with left upper lobectomy and mediastinal lymph node dissection from stations 5, 6, 9 and 10. The patient was hospitalized in the intensive care unit (ICU) of our hospital for the first 24 hours past fully conscious surgery. His post-operative recovery was uneventful and was discharged on the 8th post-operative day.
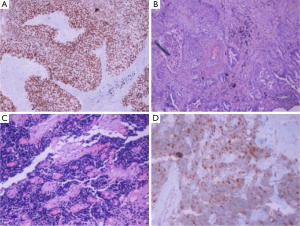
Pathologic examination of the left upper lobe revealed two lesions; tumor 1, measured 6 cm in size, was confirmed to be a squamous cell carcinoma with low differentiation; tumor 2, 1 cm away from the first tumor, measured 0.5 cm in size, was identified as adenosquamous carcinoma with moderate differentiation. Immunohistochemical staining for tumor 1 showed strong positivity for cytokeratin (CK) 5/6 and p63 (Figure 2A), focal positivity for CK 7, while it was negative for thyroid transcription factor-1 (TTF-1), CK 20, chromogranin and synaptophysin. Tumor 2 matched the morphological characteristics of squamous carcinoma along with those of adenocarcinoma at about 10% (Figure 2B). Subaortic and aortopulmonary window lymph nodes were positive for small cell lung cancer (SCLC) (Figure 2C). Immunohistochemical staining was positive for low molecular weight CK, CK 7, chromogranin, CD56, p63 and TTF-1 (Figure 2D), weakly positive for synaptophysin and CK 5/6, while ki-67 was positive in almost 100% of the neoplasmatic cells. Pulmonary ligament and hilar lymph nodes were negative for metastasis. It is worth mentioning that the entire lobe was examined thoroughly under microscopic observation to exclude any potential SCLC component.
The Thoracic Oncology Board of our hospital discussed the patient’s case, in order to determine the therapeutic plan that should be followed. Concurrent chemotherapy for SCLC with mediastinal radiation was decided. The patient started chemotherapy, with a plan of cisplatin 80 mg/m2 IV on day 1, plus etoposide 100 mg/m2 IV on days 1-3 every 28 days for 4 cycles, while radiation started along with cycle 2 of chemotherapy.
Discussion
Multiple primary lung cancers (MPLCs) can be either synchronous, or metachronous (6). Synchronous MPLC refer to two or more neoplasms that develop independently during the same period, without the involvement of common lymphatics (2). SMPLCs represent 19.6-40% of multiple lung cancer (MLC) patients, while 48.7% of patients with SMPLC have different histologic types. Whatever the type of SMPLC though, reports indicate that the 5-year survival rates are not correlated with similar or different histologic classification (6). Squamous cell carcinoma is the most common type of lung cancer, comprising over 70% of SMPLCs (7).
Generally accepted diagnostic criteria have been established, which include both imaging and pathological characteristics (2,3). However, the proposed criteria are not always sufficient, as SMPLCs are revealed more frequently, causing difficulties in determining the etiology of multiple malignant lung lesions. Modern imaging methods may provide valuable clues for preoperative distinction of SMP LCs from metastatic disease (2,8).
According to current reports, aggressive curative approach is the preferred strategy in dealing with SMPLCs, leading to an increase in overall survival, with 5-year rates up to 38% (5,9,10). Surgical procedures depend on the stage, the location of the tumors, and the patients’ performance status (5,10). Stereotactic radiotherapy and chemotherapy are also suggested to provide an added survival advantage (4,11).
Immunohistochemistry is the key in identifying such tumors, when preoperative diagnosis fails to contribute. Should it prove correct, a more detailed differentiation by the pathologist, using modern techniques, such as DNA studies or the p53 gene mutation, would be of great importance in the diagnosis and treatment of SMPLCs (6).
In the current study, we present the case of a 68-year-old male patient who was referred to our clinic for excision of a left upper lobe tumor, but histology revealed three different types of lung cancer (squamous, adenosquamous and SCLC). This study comes to underline the rarity of such cases, as well as the complexity of the treatment strategy that should be followed. Moreover, despite the fact that the two tumors of the excised lobe met the criteria for SMPLC, the positivity of the lymph nodes for SCLC arises questions, as no current study or guidelines exist for the treatment protocol of such cases.
In conclusion, it is quite difficult to distinguish a SMPLC from intrapulmonary metastases originating from a single pulmonary neoplasm or other neoplasms in different organs (2). Recent advances in imaging, along with careful clinical assessment can offer a valuable tool in the evaluation of SMPLCs and metastatic lesions. Therefore, we agree with Detterbeck et al. (1) that experienced multidisciplinary teams must define SMPLCs, judging and considering all information given.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Detterbeck FC, Postmus PE, Tanoue LT. The stage classification of lung cancer: Diagnosis and management of lung cancer, 3rd ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest 2013;143:e191S-210S.
- Martini N, Melamed MR. Multiple primary lung cancers. J Thorac Cardiovasc Surg 1975;70:606-12. [PubMed]
- Antakli T, Schaefer RF, Rutherford JE, et al. Second primary lung cancer. Ann Thorac Surg 1995;59:863-6; discussion 867. [PubMed]
- Griffioen GH, Lagerwaard FJ, Haasbeek CJ, et al. Treatment of multiple primary lung cancers using stereotactic radiotherapy, either with or without surgery. Radiother Oncol 2013;107:403-8. [PubMed]
- Finley DJ, Yoshizawa A, Travis W, et al. Predictors of outcomes after surgical treatment of synchronous primary lung cancers. J Thorac Oncol 2010;5:197-205. [PubMed]
- Riquet M, Cazes A, Pfeuty K, et al. Multiple lung cancers prognosis: what about histology? Ann Thorac Surg 2008;86:921-6. [PubMed]
- Ferguson MK. Synchronous primary lung cancers. Chest 1993;103:398S-400S. [PubMed]
- Xue X, Xue Q, Wang N, et al. Early clinical diagnosis of synchronous multiple primary lung cancer. Oncol Lett 2012;3:234-7. [PubMed]
- De Leyn P, Moons J, Vansteenkiste J, et al. Survival after resection of synchronous bilateral lung cancer. Eur J Cardiothorac Surg 2008;34:1215-22. [PubMed]
- Tanvetyanon T, Finley DJ, Fabian T, et al. Prognostic factors for survival after complete resections of synchronous lung cancers in multiple lobes: pooled analysis based on individual patient data. Ann Oncol 2013;24:889-94. [PubMed]
- Trousse D, Barlesi F, Loundou A, et al. Synchronous multiple primary lung cancer: an increasing clinical occurrence requiring multidisciplinary management. J Thorac Cardiovasc Surg 2007;133:1193-200. [PubMed]


