Editors’ note:
Over the last 3 decades, the dedication and commitment to improving the health care in China has resulted in significant improvements in the quality of both clinical practice and research. The system of medical education, however, has not evolved and improved at the same pace. In this column, the Journal analyzes the difference in medical education between the East and West. We would like to introduce the U.S. medical education system and share the excellent experience from Duke University Medical Center, including participating in the educational process as the 2015-2016 American Association for Thoracic Surgery Evarts A. Graham Travelling Fellow. We hope that the series would be suggestive and helpful to the readers.
Yaxing Shen, MD; Thomas A. D’Amico, MD
A primer on medical education in the United States through the lens of a current resident physician
Physicians are privileged to hold one of the most trusted and respected occupations worldwide. Patients depend on our competence, skills, knowledge, empathy, and professionalism as we address health issues ranging from minor problems to matters of life and death. They rely on our education and experience when they are at their most vulnerable. Despite the significant responsibilities incumbent on our profession, standards vary widely for medical training and licensure across the globe. For example, a bachelor’s degree is a prerequisite for attending medical school in the United States (US), but undergraduate medical education begins after secondary school in most countries. Passing one or more national licensure exams is not universally required to practice medicine. A period of specialty clinical training after obtaining a medical degree is recommended but not mandatory to independently practice medicine in some countries, and the duration of this postgraduate training can range from 1 year to approximately 1 decade depending on locale and specialty. The elaborate physician training process in the US can be difficult to understand for allied healthcare professionals and for physicians visiting from other countries or foreign medical graduates seeking medical licensure in the US. A basic overview of the medical education system in the US is provided below in conjunction with my personal experiences as a resident physician navigating this system.
Medical school admission in the US requires an undergraduate bachelor’s degree, typically obtained through 4 years of coursework after high school. This degree can be in any field, however prerequisite classes include biology, inorganic and organic chemistry, mathematics, physics, and English. The attrition rate among “pre-medical” students in the US has been estimated at greater than 50%, largely attributed in recent years to negative experiences with required courses (1,2). Students must also pass the Medical College Admission Test (MCAT), an all-day examination that assesses basic knowledge of biology, chemistry, and physics as well as critical analysis and reasoning skills. This exam was restructured in 2015 to include testing of social science-derived competencies in response to increasing recognition of the importance of social, psychological, and behavioral factors in healthcare outcomes and the doctor-patient relationship. Students commonly pay more than $2,000 on MCAT preparatory courses, indicative of the importance of MCAT score for entrance into most top medical schools. Notably, MCAT scores and medical school admissions have been highly correlated with socioeconomic status (3). In 2005, fewer than 10% of students entering US medical schools were from families in the two lowest quintiles of household income (4). The Association of American Medical Colleges (AAMC) has recognized the need to increase socioeconomic diversity of students entering the medical profession, and efforts are ongoing to achieve this goal (5). However, the socioeconomic profile of medical students may also reflect the high cost of medical education in the US. The median cost of attending 4 years of medical school for the class of 2015 was $226,447 for public schools and $298,538 for private schools (6). The median educational debt for indebted medical school graduates in 2014 was $178,046 based on the 2014 Medical School Graduation Questionnaire administered by the AAMC (7).
Admission to one of the 141 accredited allopathic medical schools granting a Doctor of Medicine (MD) degree in the US is highly competitive, with an acceptance rate of approximately 44% (8). The average grade point average (GPA) for matriculants to US allopathic medical schools in 2014 was 3.69 out of 4.0, vs. 3.55 for all applicants. The average MCAT score was 31.4 out of a maximum score of 45, compared to an average of 28.6 for all applicants in 2014. Attending an osteopathic medical college, which confers a Doctor of Osteopathic Medicine (DO) degree, is an alternative route to becoming a physician in the US. Currently approximately 20% of medical students in the US are enrolled in osteopathic medical schools, which provide training in osteopathic manipulative treatment and tend to emphasize holistic patient care more than allopathic medical schools. Aside from grades and MCAT scores, medical school acceptance is based on a variety of factors including letters of recommendation, a personal statement, admission interviews, and personal experiences including volunteering, research and leadership activities. “Resume-building” for medical school applications often begins in high school and continues throughout college. Obtaining a Medical Services volunteer position at my undergraduate institution was so prized that I camped outside overnight among a line of premedical students during my first month of college to ensure that I could gain healthcare and community service experience starting my freshman year. I was also one among many premedical students seeking the opportunity to engage in research during college. Three years working in a genetics laboratory with fruit flies alongside graduate students and my favorite professor sparked a passion for research that led me to question whether I wanted to become a physician or a biomedical researcher. Fortunately, I learned from my premedical advisor that both were possible and could be facilitated by entering a dual degree MD/Doctor of Philosophy (PhD) program. MD/PhD programs, also known as Medical Scientist Training Programs (MSTP), are offered by most medical schools. Forty-five programs are federally funded to provide trainees with tuition and stipend support during their extended educational period, which generally lasts 7-8 years.
Medical schools in the US typically have a 4-year curriculum, divided into 2 years of basic science coursework and 2 years of clinical clerkships. The initial 2 years are generally spent in the classroom learning biochemistry, molecular biology, physiology, gross anatomy, histology, microbiology, immunology, neurobiology and pathology. Most institutions also incorporate some interaction with patients into these first 2 years, along with instruction on the patient-doctor relationship, effective communication, humanism and professionalism. Numerous grading systems are employed throughout the US, however there has been a recent trend towards a Pass/Fail or Honors/Pass/Fail grading system rather than numerical or letter grades for pre-clerkship courses (9,10). Basic science knowledge from these first 2 years of medical school is tested by the US Medical Licensing Exam (USMLE) Step 1. A passing score on this 1-day, multiple-choice exam is required to submit an application for post-graduate clinical training (“residency”), and the Step 1 score can impact a student’s prospects of obtaining a competitive residency position.
The third year of medical school is traditionally comprised of several required core clinical clerkships. These include Internal Medicine (average 10 weeks), Surgery (average 8 weeks), Pediatrics (average 7 weeks), Obstetrics & Gynecology (average 6.5 weeks), Family Medicine (average 6 weeks), and Psychiatry (average 5.5 weeks) (11). Many schools also require clerkships in Neurology, Radiology, Emergency Medicine, and Critical Care to be performed during the third or fourth year of medical school. During these clerkships, medical students are primarily embedded within an inpatient rounding team, working closely with resident physicians and an attending physician. On average, medical students work with 1-4 patients at a time. They perform the admission history and physical examination and follow-up with their patients daily, including formulating a basic management plan, presenting patient updates on rounds, and writing progress notes. Some clerkships, such as Family Medicine, are based in part or entirely in the ambulatory care setting. This provides the opportunity for students to develop their medical interview, physical exam, and management skills for less acute medical issues in the more confined timeframe of a 10-30 min outpatient visit.
The fourth year of medical school involves additional clinical clerkships, lasting an average of 4 weeks per rotation. Fourth year students have significant flexibility in selection of these clerkships, allowing experience in subspecialty fields, consult services, and outpatient clinics. A universally required component of the fourth year is the “sub-internship” (often abbreviated “sub-I”) or “acting internship.” The medical student fills the role of an intern, which is the term for a first year medical graduate [also known as postgraduate year 1 (PGY-1)] in the US. Sub-internships are performed in Internal Medicine, Surgery, Pediatrics, or Obstetrics and Gynecology, as appropriate for the student’s planned postgraduate specialty training. The sub-intern is the primary point person on the medical team for up to four patients but works under close supervision by a senior resident and attending physician. During sub-internship, fourth year medical students are responsible for documenting notes in the medical record, performing procedures, writing medical orders, presenting on rounds, and communicating with other services and allied health professionals for their patients. Letters of recommendation for residency programs are often based on performance in this role in which students have greater autonomy and responsibility compared to other medical school clerkships. Some students will complete multiple sub-internships, including rotations at other institutions where they may wish to obtain a residency position.
Two medical licensing exams, USMLE Step 2 Clinical Knowledge (CK) and Step 2 Clinical Skills (CS), are taken during the fourth year of medical school. USMLE Step 2 CK is a multiple-choice exam assessing medical knowledge primarily through case-based questions. Step 2 CS is a one-day test in which examinees interact with twelve standardized patients and document pertinent findings, differential diagnosis, and next steps in management for each case. While the other medical licensing exams are graded on a numerical scale, Step 2 CS is scored as Pass/Fail based on the examinee’s spoken English proficiency, communication and interpersonal skills (assessed by each standardized patient), as well as appropriate workup and documentation for the clinical encounter. International medical graduates are required to pass USMLE Step 1, Step 2 CS, and Step 2 CK in order to obtain certification by the Educational Commission for Foreign Medical Graduates. This certification must be achieved by foreign medical graduates in order to take the final medical licensing exam (Step 3) and to obtain a medical license in the US. USMLE Step 3 is a 2-day, multiple-choice exam that assesses application of clinical science to the practice of medicine. This examination is usually taken towards the end of PGY-1 or during PGY-2.
Numerous medical schools in the US have recently been moving away from the traditional 4-year curriculum, for example offering a 3-year MD program (12-15). My experience also differed from the typical timeline discussed above due to the unique curriculum where I obtained my undergraduate medical education. This curriculum condenses the first 2 years of basic and clinical science classroom-based learning into 1 year. I was nervous about whether I would be able to absorb the necessary material in this shortened timeframe. Fortunately, I felt prepared and excited to move onto direct patient care after being in the classroom for 4 years of college and 1 year of medical school. The second year of medical school encompasses the basic core clinical clerkships, equivalent to the third year at most other institutions. The compressed classroom time allows students to have a full year for scholarly activity during their third year. This time is typically spent performing basic science or clinical research. Pursuit of a second degree is also common. Many of my classmates were enrolled in dual degree programs, for example obtaining a Master of Public Health (MPH) or Master of Business Administration (MBA) degree in conjunction with a MD. Other MD/PhD students and I enrolled in graduate school classes and rotated through laboratories to select a mentor with whom we would perform research over the next few years, culminating in a dissertation. The “third year” thus ranges from one to several years for students at this institution, while the fourth year is equivalent to other medical schools.
I returned for my final year of medical school with a new group of classmates after 5 years of cancer research in the Department of Pathology. I was pleasantly surprised at the relative ease of transitioning back into the world of clinical medicine. The most difficult adjustment of re-entering medical school was the stressful process of applying to residency programs in parallel with completing fourth year clerkships. Residency applications for one or more medical specialties are submitted online to multiple institutions through the Electronic Residency Application Service (ERAS) during the summer. The application includes a personal statement, list of extracurricular activities (volunteering, leadership roles, etc.), research projects and publications, USMLE score(s), medical school transcripts, and several letters of recommendation. Based on this application, residency programs invite a subset of applicants for an in-person interview.
Medical students spend a significant portion of time traveling to residency interviews between October and January of their senior year. Residency placement is assigned through “the Match”, a computerized national system managed by the National Resident Matching Program (NRMP). Residency program directors submit a rank ordered list of applicants who interviewed for a position in their program. Similarly, applicants submit a list of programs where they interviewed in order of preference. The typical number of programs ranked varies by specialty. In 2014 the median number of contiguous ranks by US senior medical students ranged from 9-15 for those who matched vs. 2-8 for applicants who did not match (16). After applicant credentials are verified, a computer algorithm attempts to match each applicant to the program most preferred on his or her list. A tentative match is made if a given program also ranked that applicant and either has an unfilled position or the applicant is more preferred by that program than an applicant with a tentative match to that program. If an applicant is displaced from a tentative match, then another attempt is made to match that applicant starting with the programs at the top of his or her rank order list. Matches are finalized once all applicant lists have been considered. Notably, match commitments are binding for the applicant and residency programs. A similar matching algorithm is used in the United Kingdom for physicians applying for specialty medical training. However, applicants in this system have 48 hours to respond to an offer, and they can continue to respond to “upgrade” offers from programs higher on their match list for a specified time period (17).
Certain specialties, such as Neurosurgery, are particularly competitive with more than 1.5 applicants for every available residency position. Furthermore, students matching in these competitive fields typically have significantly higher USMLE scores and grades, as well as more research experience compared to the average applicant (16). Students interested in these fields will often apply for a position in two specialties in case they do not match in their preferred specialty. In addition, some fields require a separate match for internship, the first year of postgraduate training. These specialties include Radiology, Neurology, Anesthesiology, Ophthalmology, Radiation Oncology, and Dermatology. I applied for residency in Radiation Oncology, which has become an increasingly competitive specialty over approximately the past 15 years (16,18). I recall having immense anxiety about whether I would obtain a match in my desired field. It seemed unfair that after so many years dedicated to study, I might not have the opportunity to practice medicine in the specialty of my choosing. On the other hand, I felt some guilt about my selection, given that the trend of residency applications favoring subspecialty fields contributes to growing unmet healthcare needs in primary care fields in the US (19-23).
I applied to more than 30 Radiation Oncology Residency Programs to maximize my chances of obtaining a match, and I was fortunate to be offered interviews at many of these programs. After researching the average number of interviews for applicants successfully matching in Radiation Oncology, I selected nine programs at which to interview. I took notes at each institution and eventually created a spreadsheet of pros and cons to help formulate my rank list. I interviewed at twice as many Internal Medicine and Transitional Year internship programs in an effort to match at internship and residency programs located in the same city. I spent thousands of dollars and accumulated many gray hairs through the residency application process, which culminated in Match Day. This is a day in mid-March when residency placement results are released nationwide. Ceremonies occur at medical schools throughout the country celebrating this rite of passage. Each graduating senior in my class was called forward in random order to pick up a sealed envelope. We each placed a dollar in a jar, and the last person to be called received this pool of money. Then we opened our envelopes in unison to learn where we would spend several years for the next stage of our medical training. I cried with joy as I called my parents to inform them that I had matched at my top choice. With my fears about the Match abated, I moved on to worrying about this daunting next phase—trading in the short white coat of a medical student for the long white coat of a physician with all of its accompanying responsibilities.
Internship and residency experiences vary widely depending on specialty, institution, location, individual personality, and numerous other factors. However, this phase of clinical training is generally recognized as a challenging period in which new physicians grapple with longer work hours, higher expectations, and a greater level of responsibility. Interns, or first year post-graduate physicians, transition within weeks from caring for four or fewer patients as a medical student to being the primary point person for up to ten patients. They are the main physician entering orders, performing clinical documentation, and communicating with patients, families, and other healthcare team members. Interns are the first person called when any issue arises for a patient. This translates to constant interruptions by a pager in the midst of writing notes, interviewing and examining patients, presenting on rounds, performing procedures, and speaking with other healthcare providers about patient issues. One of my attending physicians describes the intern role as being “everything to everyone”—including patients and their families, nurses, discharge planners, attending physicians, and so the list continues. This position forces new doctors to climb a steep learning curve, quickly moving closer to becoming an independently practicing physician. It is a worthwhile journey, and I still marvel at how much I learned during my internship year. Unfortunately, this process can take its toll emotionally and physically on new physicians in training, resulting in high rates of burnout and concerns regarding patient safety (24-27).
The Accreditation Council for Graduate Medical Education (ACGME) introduced two major work hour reforms in recent years in an effort primarily to improve patient safety with a potential secondary benefit for resident well-being. The 2003 regulations mandated that residents work a maximum of 80 hours per week averaged over 4 weeks and remain on-site for clinical duties for a maximum of 24 consecutive hours. Mandatory duty-free intervals were added, including a minimum of ten hours off between work periods, and at least one 24-hour period off duty per week averaged over 4 weeks. Further work hour restrictions were added in 2011, including reduction of duty hours to 16 hours per day for interns to eliminate the traditional 24-hour period on-call for first year trainees (28,29). Most current residents have heard attending physicians discuss “the old days” when residents essentially lived at the hospital. These stories seem to imply that current residents have “gone soft,” an attitude which is reflected in numerous surveys and commentaries that equate new duty hours with poor work ethic and decreased professionalism (30-35). However, an alternate view is that duty hour regulations compress the time that residents have to complete their work and to develop as a physician (36).
As an intern, I certainly felt pressure to leave by the 16-hour mark due to concerns that I may appear inefficient or cause my program to receive citations for duty hour violations. However, I often found it difficult to finish the necessary clinical documentation while still spending adequate time with patients to build rapport, empathize, and effectively communicate about their disease and management plans. I have observed other trainees struggle with similar conflicts between abiding by duty hour regulations and being the physician who they want to be. There is likely no easy answer to this issue, but debate continues in the US regarding the ideal way to approach duty hour requirements while maximizing patient safety and resident education (37-39). Unfortunately, most studies have not shown duty hour reforms to be associated with reduced medical errors or improved resident well-being, as demonstrated by a systematic review in 2014 by Ahmed et al. (40) and numerous recent articles (41-44). In fact, several studies have indicated an association between duty hour restrictions and worse patient outcomes (40,45-47). Furthermore, suicides by medical students and residents in the US remain too common an occurrence. Among medical trainees responding to a survey in 2003-2004, 5.7% reported suicidal ideation (48). This issue has recently garnered attention in the lay media after two residents in New York committed suicide in August 2014, and many more cases likely go unreported (49-51). There is a growing movement promoting resilience training for residents and shifting aspects of the medical culture that may contribute to resident burnout.
I am currently in my fourth year of postgraduate training and third year of residency in Radiation Oncology. Duty hour violations are a rare occurrence in this field, which is primarily based in the outpatient setting. As I have progressed through residency, I have enjoyed gradually increasing levels of responsibility and autonomy within the safe network of supervision by attending physicians. Each patient and each radiation treatment plan provides a unique learning experience. Most residency programs also incorporate didactic time into the curriculum. For example, I attended a daily lecture at noon during internship in Internal Medicine, and residents in my current program have 1 hour together each morning dedicated to reviewing various clinical topics. The ACGME also requires residents in many specialties to maintain a secure case log to track trainee involvement in various procedures, monitoring compliance with specialty-specific minimum requirements.
Upon successful completion of residency training, physicians are eligible to apply for a full medical license. This replaces the trainee license, which allows only limited medical practice under supervision of an attending physician. Many fields also require a fellowship after residency for sub-specialty training. Fellowship typically entails research time in addition to patient care-based clinical training. The duration of postgraduate clinical training varies widely for different medical specialties in the US (Table 1). After completing residency or fellowship training, physicians are Board Eligible for between 3 and 7 years depending on their specialty (52). Obtaining Board Certification is a voluntary process that is separate from medical licensure and includes one or more examinations administered by the given specialty’s Member Board within the American Board of Medical Specialties.
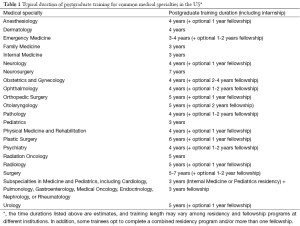
Full table
The American medical education process is complex with many facets differing from physician training processes in other countries. In my experience as a medical trainee in the US, the road to becoming an attending physician is a long but gratifying one, encompassing years of classroom study and clinical training punctuated by myriad exams for quality assurance along the way.
Acknowledgements
None.
Footnote
Conflicts of Interest: The author has no conflicts of interest to declare.
References
- Lin KY, Parnami S, Fuhrel-Forbis A, et al. The undergraduate premedical experience in the United States: a critical review. Int J Med Educ 2013;4:26-37. [PubMed]
- Drew C. Why Science Majors Change Their Minds (It’s Just So Darn Hard). The New York Times. 2011 Nov 4. Available online: http://www.nytimes.com/2011/11/06/education/edlife/why-science-majors-change-their-mind-its-just-so-darn-hard.html?_r=0
- Grbic D, Jones DJ, Case ST. Effective Practices for Using the AAMC Socioeconomic Status Indicators in Medical School Admissions. Association of American Medical Colleges. March 1, 2013. Available online: https://www.aamc.org/download/330166/data/seseffectivepractices.pdf
- Jolly P. Diversity of U.S. Medical Students by Parental Income. Association of American Medical Colleges 2008;8. Available online: https://www.aamc.org/download/102338/data/aibvol8no1.pdf
- Association of American Medical Colleges. Diversity Policy and Programs: Who We Are, What We Do, Where We’re Going. [Accessed October 4, 2015]. Available online: https://www.aamc.org/download/368724/data/dppbriefingbook20132.pdf
- Association of American Medical Colleges. Medical Student Education: Debt, Costs, and Loan Repayment Fact Card. October 2014. [Accessed October 4, 2015]. Available online: https://www.aamc.org/download/152968/data/debtfactcard.pdf
- Association of American Medical Colleges. Medical School Graduation Questionnaire: 2014 All Schools Summary Report. July 2014. [Accessed October 4, 2015]. Available online: https://www.aamc.org/download/397432/data/2014gqallschoolssummaryreport.pdf
- Association of American Medical Colleges. Applicants and Matriculants Data. [Accessed October 4, 2015]. Available online: https://www.aamc.org/data/facts/applicantmatriculant/
- Association of American Medical Colleges. Number of Medical Schools Using Selected Grading Systems. [Accessed October 5, 2015]. Available online: https://www.aamc.org/initiatives/cir/406418/11.html
- Spring L, Robillard D, Gehlbach L, et al. Impact of pass/fail grading on medical students’ well-being and academic outcomes. Med Educ 2011;45:867-77. [PubMed]
- Association of American Medical Colleges. Average Number of Required Weeks by Discipline. [Accessed October 5, 2015]. Available online: https://www.aamc.org/initiatives/cir/426810/05d.html
- Emanuel EJ, Fuchs VR. Shortening medical training by 30%. JAMA 2012;307:1143-4. [PubMed]
- Grady D. The Drawn-Out Medical Degree. The New York Times. 2014 Aug 1. [Accessed October 4, 2015]. Available online: http://www.nytimes.com/2014/08/03/education/edlife/the-drawn-out-medical-degree.html
- Boodman SG. Medical school done faster. The Washington Post. 2014 Jan 13. [Accessed October 5, 2015]. Available online: https://www.washingtonpost.com/national/health-science/medical-school-done-faster/2014/01/13/4b6d9e54-5c40-11e3-be07-006c776266ed_story.html
- Moore JD, Jr. 3-Year Curriculum: The Cure for Med-Ed’s Ills?—Words of caution about intensified programs from a veteran of one. MedPage Today. 2015 May 3. [Accessed October 5, 2015]. Available online: http://www.medpagetoday.com/PublicHealthPolicy/MedicalEducation/51339
- Charting Outcomes in the Match: Characteristics of Applicants Who Matched to Their Preferred Specialty in the 2014 Main Residency Match. 5th Edition. Washington, DC: National Resident Matching Program, 2014. Available online: http://www.nrmp.org/wp-content/uploads/2014/09/Charting-Outcomes-2014-Final.pdf
- Specialty Recruitment Applicant Handbook 2015. [Accessed October 5, 2015]. Available online: http://specialtytraining.hee.nhs.uk/files/2014/11/Applicant-Handbook-2015v4.pdf
- Wilson LD, Haffty BG. Evaluation of the National Resident Matching Program (NRMP) radiation oncology data (1993-2003). Int J Radiat Oncol Biol Phys 2003;57:1033-7. [PubMed]
- IHS Inc. The Complexities of Physician Supply and Demand: Projections from 2013 to 2025. [Accessed October 4, 2015]. Available online: https://www.aamc.org/download/426242/data/ihsreportdownload.pdf?cm_mmc=AAMC-_-ScientificAffairs-_-PDF-_-ihsreport
- Petterson SM, Liaw WR, Tran C, et al. Estimating the residency expansion required to avoid projected primary care physician shortages by 2035. Ann Fam Med 2015;13:107-14. [PubMed]
- Newton DA, Grayson MS. Trends in career choice by US medical school graduates. JAMA 2003;290:1179-82. [PubMed]
- Jeffe DB, Andriole DA, Hageman HL, et al. The changing paradigm of contemporary U.S. allopathic medical school graduates’ career paths: analysis of the 1997-2004 national AAMC Graduation Questionnaire database. Acad Med 2007;82:888-94. [PubMed]
- Jeffe DB, Whelan AJ, Andriole DA. Primary care specialty choices of United States medical graduates, 1997-2006. Acad Med 2010;85:947-58. [PubMed]
- Goldman ML, Shah RN, Bernstein CA. Depression and suicide among physician trainees: recommendations for a national response. JAMA Psychiatry 2015;72:411-2. [PubMed]
- Dyrbye LN, West CP, Satele D, et al. Burnout among U.S. medical students, residents, and early career physicians relative to the general U.S. population. Acad Med 2014;89:443-51. [PubMed]
- Resident Duty Hours: Enhancing Sleep, Supervision, and Safety. Institute of Medicine, 2008. [Accessed October 4, 2015]. Available online: https://iom.nationalacademies.org/~/media/Files/Report%20Files/2008/Resident-Duty-Hours/residency%20hours%20revised%20for%20web.pdf
- Dimitris KD, Taylor BC, Fankhauser RA. Resident work-week regulations: historical review and modern perspectives. J Surg Educ 2008;65:290-6. [PubMed]
- Resident Duty Hours in the Learning and Working Environment Comparison of 2003 and 2011 Standards. [Accessed October 5, 2015]. Available online: https://www.acgme.org/acgmeweb/Portals/0/PDFs/dh-ComparisonTable2003v2011.pdf
- Frequently Asked Questions: ACGME Common Duty Hour Requirements. [Accessed October 5, 2015]. Available online: https://www.acgme.org/acgmeweb/Portals/0/PDFs/dh-faqs2011.pdf
- Larriviere D. Duty hours vs professional ethics: ACGME rules create conflicts. Neurology 2004;63:E4-5. [PubMed]
- Ginsburg S. Duty hours as viewed through a professionalism lens. BMC Med Educ 2014;14 Suppl 1:S15. [PubMed]
- Van Eaton EG, Horvath KD, Pellegrini CA. Professionalism and the shift mentality: how to reconcile patient ownership with limited work hours. Arch Surg 2005;140:230-5. [PubMed]
- Szymczak JE, Brooks JV, Volpp KG, et al. To leave or to lie? Are concerns about a shift-work mentality and eroding professionalism as a result of duty-hour rules justified? Milbank Q 2010;88:350-81. [PubMed]
- Rybock JD. Residents’ duty hours and professionalism. N Engl J Med 2009;361:930-1. [PubMed]
- Rosenbaum JR. Can residents be professional in 80 or fewer hours a week? Am J Med 2004;117:846-50. [PubMed]
- Sen S, Nichols B, Didwania AK. Duty hour reform: only a small piece of a larger problem--reply. JAMA Intern Med 2013;173:1844-5. [PubMed]
- Arrighi JA, Hebert JC. Duty hour requirements: time for a new approach? JAMA 2014;312:2342-4. [PubMed]
- Weinstein DF, Arora V, Drolet B, et al. Residency training--a decade of duty-hours regulations. N Engl J Med 2013;369:e32. [PubMed]
- Peets A, Ayas NT. Restricting resident work hours: the good, the bad, and the ugly. Crit Care Med 2012;40:960-6. [PubMed]
- Ahmed N, Devitt KS, Keshet I, et al. A systematic review of the effects of resident duty hour restrictions in surgery: impact on resident wellness, training, and patient outcomes. Ann Surg 2014;259:1041-53. [PubMed]
- Rajaram R, Chung JW, Jones AT, et al. Association of the 2011 ACGME resident duty hour reform with general surgery patient outcomes and with resident examination performance. JAMA 2014;312:2374-84. [PubMed]
- Lee MJ. On Patient Safety: Have The ACGME Resident Work Hour Reforms Improved Patient Safety? Clin Orthop Relat Res 2015;473:3364-7. [PubMed]
- Patel MS, Volpp KG, Small DS, et al. Association of the 2011 ACGME resident duty hour reforms with mortality and readmissions among hospitalized Medicare patients. JAMA 2014;312:2364-73. [PubMed]
- Scally CP, Ryan AM, Thumma JR, et al. Early impact of the 2011 ACGME duty hour regulations on surgical outcomes. Surgery 2015. [Epub ahead of print]. [PubMed]
- Vadera S, Griffith SD, Rosenbaum BP, et al. National Incidence of Medication Error in Surgical Patients Before and After Accreditation Council for Graduate Medical Education Duty-Hour Reform. J Surg Educ 2015. [Epub ahead of print]. [PubMed]
- Babu R, Thomas S, Hazzard MA, et al. Worse outcomes for patients undergoing brain tumor and cerebrovascular procedures following the ACGME resident duty-hour restrictions. J Neurosurg 2014;121:262-76. [PubMed]
- Babu R, Thomas S, Hazzard MA, et al. Morbidity, mortality, and health care costs for patients undergoing spine surgery following the ACGME resident duty-hour reform: Clinical article. J Neurosurg Spine 2014;21:502-15. [PubMed]
- Goebert D, Thompson D, Takeshita J, et al. Depressive symptoms in medical students and residents: a multischool study. Acad Med 2009;84:236-41. [PubMed]
- Sinha P. Why Do Doctors Commit Suicide? The New York Times. 2014 Sep 4. Available online: http://www.nytimes.com/2014/09/05/opinion/why-do-doctors-commit-suicide.html
- Oaklander M. Life support: Inside the movement to save the mental health of America’s doctors. Time Magazine 2015 August 27:42-51. Available online: http://time.com/4012840/doctors-on-life-support/
- McPartland AS. Suicide and the Young Physician. The Atlantic. 2014 September 16. Available online: http://www.theatlantic.com/health/archive/2014/09/suicide-and-the-young-physician/380253/
- American Board of Medical Specialties. ABMS Board Eligibility Policy. [Accessed October 5, 2015]. Available online: http://www.abms.org/board-certification/board-eligibility/


