
Cosmetic male genital surgery: a narrative review
Introduction
Since Antiquity, the penile size has been a significant issue for men (1). Some men experience distress either due to having micropenis or even with average-sized penis (2). As it’s often the case in aesthetic surgery this distress must be separate from penile dysmorphic disorder (PDD) or small penis anxiety (SPA), that are included within the body dysmorphic disorder (BDD) spectrum in the Diagnostic and Statistical Manual of Mental Disorder, fifth edition (3). Worldwide, penile enhancement has become the second most desired aesthetic operation in men, according to the International Society of Aesthetic Plastic Surgery (ISAPS) Global Survey 2018. This narrative review aims to describe and critically discuss male intimate cosmetic surgeries. We present this article in accordance with the Narrative Review reporting checklist (available at https://atm.amegroups.com/article/view/10.21037/atm-23-351/rc).
Methods
We performed a narrative review of the literature using PubMed from January 2000 to September 2022. The author (M.A.D.) and an experienced co-researcher (R.L.) designed and conducted the search strategy independently. The search terms with different combinations include: “penile aesthetics”, “penis”, “scrotum aesthetics”, “male genitalia”, “girth thickness”, “size”, “enlargement”, “augmentation”, “aesthetic”, and “cosmetic” (Table 1). Backward chaining of reference lists from retrieved papers was also used to extend the research. The literature search was then limited to English-language publications from peer-reviewed journals with an impact factor over 0.5. Retrospective and prospective primary clinical studies were included only when performed on patients with male genital anatomy with no deformities at birth. Conference abstracts, case reports, small case series (≤10 cases), editorial comments, letters to the editor, brief communications, and animal studies were withdrawn.
Table 1
| Items | Specification |
|---|---|
| Date of search | 15th September, 2022 |
| Databases and other sources searched | PubMed |
| Search terms used | “Penile aesthetics”, “penis”, “scrotum aesthetics”, “male genitalia”, “girth thickness”, “size”, “enlargement”, “augmentation”, “aesthetic”, and “cosmetic” |
| Timeframe | From January 2000 to September 2022 |
| Inclusion and exclusion criteria | Inclusion criteria: peer reviewed papers in English; impact factor >0.5 journals; retrospective and prospective primary clinical studies |
| Exclusion criteria: conference abstracts, case reports, small case series (≤10 cases), letters to the editor, brief communications, editorial comments, animal studies were excluded | |
| Selection process | Two authors (M.A.D. and R.L.) |
Selection of articles and data extraction
The article titles and the abstracts were reviewed independently by two of the authors. Identic references were discarded, and a complete review of the potentially relevant papers was accomplished using the elimination and inclusion criteria by a third author (A.D.). The following data were retrieved: year of publication, study design, the total number of patients and the number of procedures, type of technique, surgical outcomes, complications, and patient satisfaction.
Results classification
Publications have been classified according to the objectives displayed and the techniques used.
Results
The initial database search brought a total of 950 articles, and 33 additional references were further identified from these papers. After excluding identic publications, 770 articles were analyzed, leaving 180 articles in our list after applying the exclusion criteria with abstract analysis. A content analysis was then carried out, and only 24 articles were selected to create our narrative review. We separated these papers into four groups regarding the goal of the procedure: 14 articles on girth augmentation, 7 on length and girth augmentation, and 3 on scrotal enhancement (Figure 1).

Non-invasive techniques
The efficiency of penile weights, stretching, or vacuum devices, highly advertised on the internet as a non-invasive option to increase penile length, was not confirmed in our narrative literature review (4).
Non-surgical penile shaft girth augmentation
Although we did find posts on liquid silicone for non-surgical penis girth augmentation, only articles on polylactic acid, highly cohesive hyaluronic acid (HA), and penile polymethylmethacrylate-based soft tissue fillers matched our inclusion criteria (5-8). At 24 weeks, the mean penile girth increases ranged from 1 to 4 cm, with a high level of patient satisfaction and increases the satisfaction in the sexual life on a visual analog scale. There were no differences between the selected fillers. No serious adverse effects were reported apart from filler injection-related adverse events in 5% to 14% of cases. Penile surface irregularities are the most common cosmetic complication.
In our experience
This procedure can be executed in an office setting with regional bloc anesthesia by injecting lidocaine at the root of the penis. We use a highly cohesive HA injected with an 18-G blunt cannula inserted via a suprapubic approach. The filler is injected between the Dartos fascia and Buck’s fascia using the fanning technique. The volume of filler injected is usually set at 5 to 15 mL. An elastic penile support bandage is then placed for 24 hours. Antibiotics are prescribed for 3 days, and patients were asked to not have sexual intercourse for 2 weeks (Figure 2A,2B).

Non-surgical penile glans girth augmentation (9-11)
The penis is composed by two parts: the glans and shaft. Notably, the penile augmentation focused on the penile shaft. After penile shaft augmentation, the glans appeared relatively smaller, creating new imbalances in penile overall shape resulting in new self-esteem problems. In current practice, most patients seek both a penile shaft and a glans penis augmentation (GPA), if possible. An adequate substance selection is crucial for glans injections. Ideal substances for soft-tissue augmentation should maintain their volume, be safe, biocompatible, and non-migratory. Because of its highly vascularized structure, the safe space for injection into the glans penis is relatively tiny, choosing an appropriate substance is of utmost importance.
In our review, several materials for GPA with injection have been assessed, including hydrogel that included a synthetic cross-linked polymer, polyacrylamide gel and HA gel. A significant increase in the glans’ circumference was reported at a 1-year follow-up. An average of 5.6 mL was injected, in a mean procedure time of 30 minutes. The mean increase of the glans’ surface represented between 45% and 70%. GPA is associated with delayed ejaculation in several publications.
In our experience
Highly cohesive HA appeared to be effective and safe for GPA. This procedure can be performed in an office setting with regional bloc anesthesia using a lidocaine injection at the root of the penis with an additional infusion of 0.2% lidocaine underneath the coronal sulcus. HA gel is injected into the subcutaneous tissue (lamina propria layer) thanks to 24-G needles. The injection points were located at the 1 and 11 o’clock positions on the corona of the glans to avoid dorsal pedicle injury. The product was injected into the glans penis with a fan-like fashion. These needles are then directed posteriorly and laterally parallel or tangential to the glans for a uniform distribution of the material by a continuous back-and-forth movement. The total procedure time is about 30 minutes for an injection ranging from 3 to 5 mL. Our practice consists of injecting five to ten syringes (1 mL) of HA into the penis shaft. For the glans we generally inject three syringes (1 mL). The product deploys the full volume in 48 hours and the stability is from 10 to 18 months. It is therefore an injection to be repeated every year.
Surgical penile girth augmentation
Corpus cavernosum augmentation
Austoni et al. (12) established the concept of a corporoplasty with a saphenous vein graft. The graft is extended at the level of sub-albuginea cavernous tissue, thus exposed, from the base of the large body to the bottom of the glans. This is the only technique that can increase the volume of the erect penis when there is no increase in the flaccid state. The authors reported 39 patients who benefited from this procedure, with low complication rates (9%) and excellent aesthetic results. At 9 months, the diameter of the penis in erection had increased from 1.2 to 2.1 cm, and all men had regained regular sexual activity at 4 months postoperative. However, this aggressive surgery seems challenging to defend in a cosmetic surgery project.
Acellular dermal matrix (Figure 3A-3D)

We found two studies (13,14) describing the positioning of a human acellular dermal matrix allograft between the dartos fascia and the buck’s fascia. After preconditioning in normal saline for 20 minutes, mesh incisions were made in the aim to facilitating the blood flow. A complete incision was made below the coronary sulcus till the buck’s fascia. Then the dartos fascia was separated from the buck’s fascia. The prepared graft was then placed on top of the buck’s fascia. The results seem encouraging. Nevertheless, cases of skin erosion of the penile shaft, intense fibrosis, and graft infection have been reported (14).
Fat injection (Figure 4A-4C)

In our experience
Fat injection represents the gold standard. The principle consists of harvesting fat by liposuction at the abdominal, thigh or gluteal level or the level of the inner face of the thighs and reinjecting it after centrifugation in the penis sheath dartos.
We instilled the designed area of liposuction with 500 cc of a saline solution with epinephrine (1:800,000) and 0.02 xylocaine (50 cc xylocaine 1% per 1 L of solution) through the suprapubic incision using an electric device (Osseo Doc, Bienair MOT300, Clichy, France). Then, the fat was harvested thanks to a power-assisted liposuction system (MicroAire iP.A.L.TM; MicroAire Surgical Instruments LLC, Va., Charlottesville, VA, USA) using a 3-mm multiple-hole cannula attached to a handpiece and set to 0.5 bars and 0.5 atm. The fat was then treated by centrifugation at 2,000 rpm (400 G) for 2 minutes to obtain a purified fat with almost nonexistent oily supernatant, without compromising the efficiency of the graft. The nano fat graft was obtained by shifting the fat with 20-cc syringes after ten passes (15). The nano fat was reinjected through a punctiform proximal incision with a retrograde deposition from distal to proximal. A variation of this technique for penile augmentation is described by Kang et al. with a tumescent infiltration with a modified Klein’s solution into the lower abdomen or inner thighs and a purification by a centrifugation (3,000 rpm for 3 min) of the washed fat (16). Our recently published paper reported an injection from 60 to 90 mL for a median rise of 3.6 cm. The challenge of this technique consists of finding the right injection volume with minimal complications and a significant girth gain. Indeed, many adipocytes are destroyed or reabsorbed, and the result should be viewed with a loss of at least 30% of the injected volume (17). Therefore, the aesthetic result remains consistent with a significant satisfaction rate. Deformations, paraphimosis, asymmetrical deposition, nodules or granulomas constitute the corpus of complications (18).
Penile lengthening
Sliding elongation
We found two publications describing a surgical method to lengthen the corpora cavernosa by placing circumferential autologous veins or acellular dermal grafts associated with a penile implant stated by the authors, results are limited by the extensibility of the dorsal neurovascular bundle of the penis in a non-shrinking organ (19,20). The authors report an average gain in length of 3.1 cm with an average follow-up of 37 months. Due to this method’s vascular risk, it should be reserved for the treatment of Peyronie’s disease with severe curvatures, shrinkage, loss of length and erectile dysfunction.
Penile disassembly
Perovic and Djordjevic (21) describe a procedure that separates the glans cap accompanied with a neurovascular bundle dorsally, from the corpora cavernosa, and the urethra ventrally. Thus, the corpora are entirely separated from the surrounding tissues. An autologous rib cartilage graft is placed between the glans cap and the tip of the corpora cavernosa. On 19 patients, the authors found an average increased length of 3 cm. This method’s vascular and infection risks prevent it from being used in cosmetic surgery.
In our experience (18)
The suspensory ligament release represents the safest surgical technique for many patients with small penis syndrome.
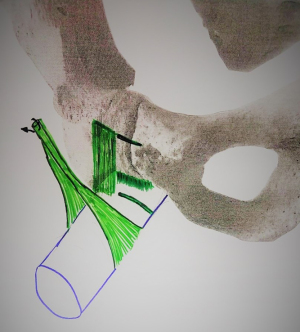
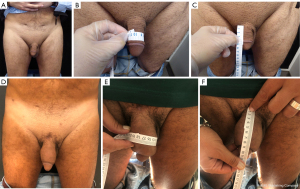
Historically anatomists like Rouviere were convinced that the penile suspensory ligament was a single structure extending from the pubic bone to the corpus cavernosum of the penis (22). The function of this ligament was historically assumed to be to stabilize the penis during erection (23). It was later demonstrated that rather than a single ligament, a whole apparatus supported and stabilized the penis (24). The segmentation of the anatomical structures of the penile suspensory device of the penis allowed us to identify four different ligaments: the fundiform ligament, the suspensory ligament, the thick vertical ligament, and the arcuate ligament (Figure 5). No role of stabilization was found for the fundiform, and suspensory ligaments, thus they could be safely released. A horseshoe pubic transverse incision right at the penopubic junction is made despite that it may result in hairless or depressed pubic areas. Moreover, the angle of erection may change. A fat flap was mobilized from the suprapubic region to the space between the pubic symphysis and corpora cavernosum, avoiding unwanted reattachment and secondary shortening. The combination with lipofilling of the penile shaft will increase the weight of the penis and maintain the length gain. The gain of penile length thanks to suspensory ligament release may vary. In our study about micropenis augmentation (18), all the measurements were carried out under the same strictly reproducible conditions: same exam room, same light, same temperature. The patient was standing and the measurements were taken after two penile stretching pulls by the patient. We reported a mean lengthening of 3.4 cm (range, 1.5–7 cm). The main procedure used in the included articles was ligamentolysis. Even though the studies reported the size of the penis pre- and postoperatively, the measurements were made with a heterogeneity in the state of the penis. The reported mean gain ranged from 1.5 to 6 cm (Figure 6A-6F).
Foreskin surgery
Its resection is a frequent request that can exist independently of phimosis. The reasons can be aesthetic, cultural, religious, and sometimes hygienic. Thirty percent of men in the world population are circumcised (25). The technique consists of a partial excision of the foreskin, comprising a distal skin collar lined with the preputial mucosa. There then persists a foreskin covering only the base of the glans (postectomy). It is also possible to perform a complete excision skin and mucous membrane of the foreskin, the glans being completely uncovered (circumcision).
Before circumcision, it’s essential to assess the skin laxity with pictures of the erect organ; following the circumcision, the skin should be utterly retractile from the glans during erection without any tension. For this purpose, it is important to excise the appropriate amount of foreskin during circumcision. On one hand, after incomplete resection, there remains a risk for inflammation, hypertrophic scar formation and even paraphimosis. On the other hand, excessive resection should be avoided because penile shortening can occur. We observed the best results with the suture line about 5 to 10 mm from the coronal sulcus.
The main complications are hypertrophic scar with or without paraphimosis, scar wrinkling, excess of the remaining foreskin with sexual dysfunction, and tight spot with no skin retraction during erection paraphimosis was diagnosed. Poor cosmetic outcomes may impair the body image and have consequences on sexual function. In the aesthetic field, the most frequent reason for revision was a too-tight scar or a keloid formation (26).
Scrotal webbing (Figure 7A-7C)

The insertion of the scrotum on the ventral aspect of the phallus, referred as scrotal webbing, can cause of an apparent small penis. In those cases, the raphe of the scrotum continues internally on the undersurface of the penis for a much greater distance than usual. Clinically, the patient presents with an apparent small phallus, but on palpation, the penile shaft will be found to be of average size and caliber. In some cases, the webbing may reach the prepuce (27,28). The penoscrotal webbing occurs regardless the circumcision status. This developmental anomaly presumably results from the failure of the scrotal swellings to shift caudally in fetal life—the penis, which then appears short and stocky. The operative technique consists of a triangular excision of the webbing with the suture extending the raphe midline of the scrotum thanks to a Z-plasty at the penoscrotal junction, preventing a scar contracture. An intracavernosal injection of prostaglandin E1 induced an artificial erection to determine the maximal amount of skin that can be removed without causing penile constriction during erection. To restore the penoscrotal border, one or two V-Y advancement flaps at the area of the penoscrotal web (29).
Scrotal lifting
Aging can result in scrotal changes, such as laxity presenting with a low-hanging scrotum and significant distention of the scrotum, which can lead to testicular hypermobility responsible for painful testicular sub-torsions like phenomenon.
The treatment consists of harmonious excision of the excess skin of the scrotum with a horizontal excision of the mid to upper scrotum. In case of asymmetry, asymmetrical excision of the lower scrotal skin may be performed. The skin with underlying dartos fascia is excised.
The closure is made by suturing the dartos with resorbable sutures and the skin with subcuticular resorbable sutures. It is important to mention that the posterior scrotum should be preserved because of its superior lymphatic drainage. The most common complication is a hematoma, hence proper hemostasis is critical (28).
Scrotox
Scrotox refers to a non-surgical cosmetic treatment of the scrotum with Botox injections. Scrotox involves having Botox injected into the testicles, more specifically injected into the cremaster muscle and Dartos muscles (30,31). This treatment can reduce the sweating, reduce the wrinkles, and make the scrotum appear larger by relaxing the muscles, hence enhance the cosmetic appearance. We mention this practice here considering its popularity, even if no article had reached the threshold for inclusion in our narrative review.
Discussion
This study described and critically discussed the current evidence about genital enhancement procedures for men. We designed a narrative review of the literature. A comprehensive search in the MEDLINE database was performed. Original articles in English-language, published until September 2022, were selected. A total of 24 studies were included covering the total spectrum of male genital aesthetic enhancement.
Here are the key findings:
- Non-invasive approaches reported a minimal, temporary and non-significant increase in penile girth and length.
- Non-surgical penile shaft and glans augmentation with highly cohesive HA fillers gives a high level of patient satisfaction at 24 weeks and will last for 10 to 14 months. It increases the visual analog score on the scale for sexual life satisfaction without serious adverse events.
- Fat injection represents the gold standard for surgical penis girth augmentation. The principle consists of harvesting fat by liposuction at the abdominal, thigh or glute and reinjecting it after centrifugation in the penis sheath dartos. After a 40% initial resorption, the augmentation will be stable. The aesthetic results are consistent with a significant satisfaction rate. Deformations, infections, paraphimosis, asymmetrical deposition, nodules or granulomas constitute the corpus of complications.
- The fundiform and suspensory ligaments release via a transverse horseshoe incision just above the penopubic junction. This represents the safest surgical technique for penile elongation. It gives a significant length augmentation with minimal complications. A fat flap mobilized from the suprapubic area may be transposed in the space between the pubic symphysis and corpora cavernosum to prevent reattachment and secondary shortening. The combination with lipofilling of the penile shaft will increase the weight of the penis and also maintain the length gain. The amount of penile length gained with fundiform and suspensory ligaments’ release may vary from one patient to another.
- Foreskin and scrotal enhancement are entirely part of those patients’ demands. This surgery is an emerging aspect of genital male aesthetic surgery and should benefit more specific publications in the near future.
- Skin necrosis or ulcers, wound infections, or need for reoperation were reported at a low rate inferior to 5% in 12 of our selected studies. Patients should have this information in the informed consent process.
Conclusions
Our review highlighted the poor results associated with non-invasive techniques, the overall positive results of injection procedures and the excellent efficiency and a high satisfaction rate with a risk of complications in patients undergoing surgical treatments.
If the high satisfaction rate shows a real benefit, the complications are probably under-reported and should be scrupulously published. These procedures should be done by dedicated genital plastic surgeons or plastic urologists to be able to face potential complications.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Johnny Ionut Efanov) for the series “The Modern Plastic and Reconstructive Surgeon – Collaborator, Innovator, Leader” published in Annals of Translational Medicine. The article has undergone external peer review.
Reporting Checklist: The authors have completed the Narrative Review reporting checklist. Available at https://atm.amegroups.com/article/view/10.21037/atm-23-351/rc
Peer Review File: Available at https://atm.amegroups.com/article/view/10.21037/atm-23-351/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://atm.amegroups.com/article/view/10.21037/atm-23-351/coif). The series “The Modern Plastic and Reconstructive Surgeon – Collaborator, Innovator, Leader” was commissioned by the editorial office without any funding or sponsorship. M.A.D. is the consultant for Allergan, Johnson and Johnson, and Establishment labs and participates to the safety board of Knight therapy and Activis med. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All clinical procedures described in this study were performed in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from patients for the publication of this article and accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Johnston L, McLellan T, McKinlay A. (Perceived) size really does matter: Male dissatisfaction with penis size. Psychology of Men & Masculinity 2014;15:225-8.
- Marra G, Drury A, Tran L, et al. Systematic Review of Surgical and Nonsurgical Interventions in Normal Men Complaining of Small Penis Size. Sex Med Rev 2020;8:158-80. [Crossref] [PubMed]
- Nicewicz HR, Boutrouille JF. Body Dysmorphic Disorder. 2022. In: StatPearls. Treasure Island: StatPearls Publishing; 2023.
- Oderda M, Gontero P. Non-invasive methods of penile lengthening: fact or fiction? BJU Int 2011;107:1278-82. [Crossref] [PubMed]
- Yang DY, Ko K, Lee SH, et al. Efficacy and safety of a newly developed polylactic acid microsphere as an injectable bulking agent for penile augmentation: 18-months follow-up. Int J Impot Res 2017;29:136-41. [Crossref] [PubMed]
- Kwak TI, Oh M, Kim JJ, et al. The effects of penile girth enhancement using injectable hyaluronic acid gel, a filler. J Sex Med 2011;8:3407-13. [Crossref] [PubMed]
- Yang DY, Jeong HC, Ahn ST, et al. A Comparison Between Hyaluronic Acid and Polylactic Acid Filler Injections for Temporary Penile Augmentation in Patients with Small Penis Syndrome: A Multicenter, Patient/Evaluator-Blind, Comparative, Randomized Trial. J Sex Med 2020;17:133-41. [Crossref] [PubMed]
- Casavantes L, Lemperle G, Morales P. Penile Girth Enhancement With Polymethylmethacrylate-Based Soft Tissue Fillers. J Sex Med 2016;13:1414-22. [Crossref] [PubMed]
- Yang DY, Ko K, Lee SH, et al. Efficacy and safety of newly developed cross-linked dextran gel injection for glans penis augmentation with a novel technique. Asian J Androl 2018;20:80-4. [Crossref] [PubMed]
- Shaeer O. Shaeer's glans augmentation technique: a pilot study. J Sex Med 2012;9:3264-9. [Crossref] [PubMed]
- Moon du G. Kwak TI, Kim JJ. Glans Penis Augmentation Using Hyaluronic Acid Gel as an Injectable Filler. World J Mens Health 2015;33:50-61. [Crossref] [PubMed]
- Austoni E, Guarneri A, Cazzaniga A. A new technique for augmentation phalloplasty: albugineal surgery with bilateral saphenous grafts--three years of experience. Eur Urol 2002;42:245-53; discussion 252-3. [Crossref] [PubMed]
- Zhang H, Jin C, Zhang P, et al. Human Acellular Dermal Matrix Augmentation Phalloplasty Surgery. Plast Surg (Oakv) 2020;28:161-6. [Crossref] [PubMed]
- Bruno JJ 2nd, Senderoff DM, Fracchia JA, et al. Reconstruction of penile wounds following complications of AlloDerm-based augmentation phalloplasty. Plast Reconstr Surg 2007;119:1e-4e. [Crossref] [PubMed]
- Tonnard P, Verpaele A, Peeters G, et al. Nanofat grafting: basic research and clinical applications. Plast Reconstr Surg 2013;132:1017-26. [Crossref] [PubMed]
- Kang DH, Chung JH, Kim YJ, et al. Efficacy and safety of penile girth enhancement by autologous fat injection for patients with thin penises. Aesthetic Plast Surg 2012;36:813-8. [Crossref] [PubMed]
- Nguyen A, Pasyk KA, Bouvier TN, et al. Comparative study of survival of autologous adipose tissue taken and transplanted by different techniques. Plast Reconstr Surg 1990;85:378-86; discussion 387-9.
- Danino MA, Benkahdra M, El Khatib A, et al. Anatomical Study of the Penile Suspensory System: A Surgical Application to Micropenis. Plast Reconstr Surg Glob Open 2023;11:e4728. [Crossref] [PubMed]
- Egydio PH, Kuehhas FE, Sansalone S. Penile length and girth restoration in severe Peyronie's disease using circular and longitudinal grafting. BJU Int 2013;111:E213-9. [Crossref] [PubMed]
- Egydio PH, Kuehhas FE. Penile lengthening and widening without grafting according to a modified 'sliding' technique. BJU Int 2015;116:965-72. [Crossref] [PubMed]
- Perovic SV, Djordjevic ML. Penile lengthening. BJU Int 2000;86:1028-33. [Crossref] [PubMed]
- Rouvière H, Delmas A. Anatomie descriptive du système nerveux central. In: Rouvière H, Delmas A. Système nerveux central, voies et centres nerveux. 15th ed. Paris: Masson; 2002:84-5.
- Steiner MS. The puboprostatic ligament and the male urethral suspensory mechanism: an anatomic study. Urology 1994;44:530-4. [Crossref] [PubMed]
- Hoznek A, Rahmouni A, Abbou C, et al. The suspensory ligament of the penis: an anatomic and radiologic description. Surg Radiol Anat 1998;20:413-7. [Crossref] [PubMed]
- Morris BJ, Wamai RG, Henebeng EB, et al. Estimation of country-specific and global prevalence of male circumcision. Popul Health Metr 2016;14:4. [Crossref] [PubMed]
- Chevallier D, Haertig A, Faix A, et al. Cosmetic surgery of the male genitalia. Prog Urol 2013;23:685-95. [Crossref] [PubMed]
- Alter GJ. Correction of penoscrotal web. J Sex Med 2007;4:844-7. [Crossref] [PubMed]
- Alter GJ, Salgado CJ, Chim H. Aesthetic surgery of the male genitalia. Semin Plast Surg 2011;25:189-95. [Crossref] [PubMed]
- Chang SJ, Liu SP, Hsieh JT. Correcting penoscrotal web with the V-Y advancement technique. J Sex Med 2008;5:249-50. [Crossref] [PubMed]
- Ramelli E, Brault N, Tierny C, et al. Intrascrotal injection of botulinum toxin A, a male genital aesthetic demand: Technique and limits. Prog Urol 2020;30:312-7. [Crossref] [PubMed]
- Cohen PR. Scrotal Rejuvenation. Cureus 2018;10:e2316. [Crossref] [PubMed]


