Delayed aortic rupture following perforating trauma
Introduction
Death from rapid exsanguination is the immediate result in 90% of stab wounds to the aorta (1). Delayed aortic rupture under these circumstances is very rare. A PubMed data search found only one similar case, which was reported in 1996 (2). In our hospital, an aortic rupture was not found during an exploratory laparotomy in a patient who had an upper abdominal stab wound. However, on the fifth day following surgery, this patient died suddenly from an aortic rupture. The perforating wound of the aorta was confirmed by an exploratory laparotomy and the autopsy. This case showed that delayed aortic rupture after being stabbed by a pointed or sharp-edged instrument is possible. The detailed treatment process was reviewed, and pathophysiological causes for the delayed aortic rupture in this case were proposed for further discussion with peer specialists.
Case report
A 16-year-old male was stabbed in the upper abdominal area during a violent attack. He was admitted to our emergency operating room thirty minutes after he was injured. On admission, he was conscious but appeared anxious. He was pale and had cold sweats. The patient did not have a fever. His heart rate was 113 beats/min, his blood pressure was 94/74 mmHg, and his respiration rate was 20 breaths/min. The 2 cm-wide stab wound was 5 cm below the xiphoid process. Small discontinuous bleeding occurred, and part of the greater omentum was visible. His abdomen was soft and nondistended with an overall tenderness. The laboratory results from the emergency room indicated that everything appeared normal with the exception of the hemoglobin (Hgb) level, which was 119 g/L. The results from the B-mode ultrasound suggested the possibility of a small amount of hemoperitoneum in the retroperitoneal space adjacent to the upper pole of the right kidney. An exploratory laparotomy was immediately performed through a midline incision under general anesthesia. Approximately 500 mL of dark red blood was found in the abdominal cavity, and quite a few blood clots were found in the pelvic cavity. Total blood loss was estimated to be 2,000 mL. The liver and the spleen were not injured. No active bleeding was present in the abdominal cavity. A 2 cm tear through all layers of the stomach wall was found near the lesser curvature of the stomach. The tear presented with clean edges. Furthermore, there was no obvious leakage of stomach contents or resulting contamination. The tear was repaired using a full-thickness mattress suture technique. To enter the lesser sac, the gastrocolic ligament was divided. A 2 cm tear through all layers of the posterior gastric wall was found along the lesser curve that corresponded to the tear at the anterior gastric wall. The tear presented with clean edges, and there was no obvious leakage of stomach contents or resulting contamination. The tear was repaired using a double mattress suture technique. There was no damage found in the duodenum or more distal areas of the digestive tract.
We further investigated the possible wound tract in the lesser sac, and a 1 cm × 3 cm small retroperitoneal hematoma was found adjacent to the inner side of the uncinate process of the pancreas When opening up the retroperitoneal space adjacent to the hematoma, dark red venous blood gushed out from the inner side of the uncinate process of pancreas, and a superior mesenteric vein injury was identified. After applying pressure over the bleeding area, the vein lesion was repaired with a single layer suture technique using 3-0 Prolene sutures. No additional bleeding was found, and the hematoma stopped expanding after the procedure. There was no other hematoma found in the retroperitoneal space, and the blood supply and movement of the intestinal tract were normal. After removing the blood clots and the hematoma from the pelvic and abdominal cavities, drainage tubes were placed in the lesser sac and the pelvic cavity, and an indwelling gastric tube was applied. The abdominal closure was performed using a full-thickness retention suture technique. Nine units (U) of red blood cell suspensions were transfused during the surgery (1 U of red blood cell suspension was extracted from 200 mL of whole blood). The patient’s vital signs were stable during the surgery. After waking up from the anesthesia, he was sent to the inpatient unit for post-surgical monitoring and treatment.
After the surgery, the patient was still complaining about a discontinuous, moderate, dull pain that was located in an unidentified abdominal area. The abdominal was nondistended and soft. There was no well-defined area of tenderness. The borborygmus was normal. The cause of the abdominal pain was determined to be the surgical incision and a post-surgical intestinal spasm. The pain was alleviated using a spasmolytic and eased after four days of treatment. Following the surgery, 1,500 U of tetanus antitoxin was administered, and intravenous infusions containing antibiotics and parenteral nutrition were given. The water-electrolyte balance was adjusted according to the lab reports. Once the patient started to expel flatulence after the surgery, the gastric tube was removed, and he started taking a water and liquid diet. The amount of dark red hemorrhagic discharge from drainage tubes, which were placed in the lesser sac and pelvic cavity, decreased during the first four days after surgery, and the color turned lighter. The discharge separated into a light yellow suspension and a dark red precipitate after standing and was determined to be a mixture of peritoneal fluid and the remaining hemoperitoneum in the abdomino-pelvic cavity. The Hgb level was monitored consecutively for three days after the surgery, indicating that the patient remained slightly anemic. The red blood cell suspension transfusions were performed immediately following the surgery and again on the first day and the third day after the surgery (Table 1). The patient was stable within four days after the surgery and did not have a fever. The heart rate decreased from 110-120 beats/min to below 100 beats/min. The urine volume was 1,500-2,000 mL/day. The energy level and physical strength of the patient were improved. He was able to turn over and perform exercises in the bed, but he could not get off of the bed.
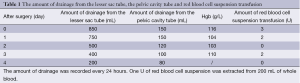
Full table
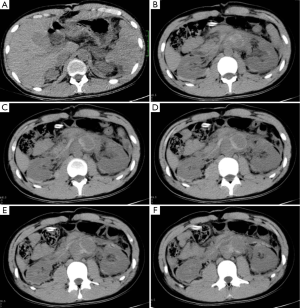
On the fourth day after the surgery, the patient underwent a plain abdominal CT scan (Figure 1). A 5 cm section of the anterior aorta located in the retroperitoneal space adjacent to the middle part of the kidney appeared structurally vague. Several hematomas and a small amount of hemoperitoneum were observed. A small amount of hemoperitoneum was also observed in the perirenal space, and a small amount of effusion was observed in the abdomino-pelvic cavity. The attending doctor believed the complications in the retroperitoneal space resulted from a superior mesenteric vein injury found in the previous exploratory laparotomy.
In the early morning on the fifth day after the surgery, the patient reported sudden, severe wrist pain on the right side. His heart rate was 105 beats/min, and his blood pressure was 100/60 mmHg. His abdomen was soft and nondistended, and no palpable mass was found. The amount of discharge from the drainage tubes did not change. The right side of the abdominal area presented with slight tenderness. The Hgb level was 108 g/L. The attending doctor determined that the pain was most likely the result of a urinary tract spasm caused by the retroperitoneal hematomas. Twenty minutes after an intramuscular injection of anisodamine, the pain was alleviated, and the patient fell asleep quietly. After four hours, the patient had sudden, severe abdominal pain. The patient was pale and had cold sweats. His heart rate was 160 beats/min, his blood pressure was 84/62 mmHg, and his respiration rate was 30 breath/min. Abdominal distension was observed. The amount of discharge from the drainage tubes did not change. The Hgb level was 62 g/L. The attending doctor determined that there was a sudden, massive bleeding in the abdominal cavity. An emergency intravenous infusion and red blood cell suspension transfusion were given. The patient was sent to the emergency room, and an exploratory laparotomy was performed under general anesthesia. The sutures were removed to re-investigate the abdominal cavity. A small amount of hemoperitoneum was found in the abdominal cavity. A dark red, massive high-pressure retroperitoneal hematoma had formed from the diaphragm to the pelvic cavity. The estimated blood loss was 3,000 mL. The crystalloid fluid, colloidal solution, and red blood cell suspension were administered to the patient in large amounts, and simultaneously, his blood pressure was maintained using drugs. An ice cap was used to protect the brain. The hematoma was then opened from side. The structure of the retroperitoneal space was already difficult to see, and massive, rapid bleeding was observed. After applying pressure on the proximal and distal areas of the abdominal aorta, a manual probing was performed. Finally, a 1 cm tear penetrating the aorta was found on both the anterior and posterior walls of the aorta adjacent to the renal arteries. At the same time, the patient’s heart beat stopped, and he did not respond to resuscitation. The patient died. The findings from the operation were confirmed by the autopsy.
Discussion
This case is unique because 1 cm-long, sharp tears were found on both the anterior and posterior walls of the aorta, but the rupture and bleeding did not occur when the patient was first injured. Additionally, no obvious bleeding was observed in the retroperitoneal space when the first exploratory laparotomy was performed. It is hard to explain this phenomenon even though the patient had lost more than 2,000 mL of blood, and as a result, his blood pressure was slightly lowered. The patient’s treatment process was reviewed, which identified a few important questions.
First of all, was it necessary to investigate the main blood vessels in the retroperitoneal space after a small retroperitoneal hematoma adjacent to the inner side of the uncinate process of the pancreas was found during the first exploratory laparotomy? According to clinical practice principles, when abdominal trauma occurs, a hematoma in the upper central retroperitoneal space may indicate important blood vessel damage. Therefore, further investigation is strongly recommended. However, the attending doctor thought the small and limited hematoma around the pancreas could be explained as the result of bleeding from the superior mesenteric vein injury. The bleeding stopped after using a single layer suture technique, and the hematoma did not expand. There were no other hematomas or bleeding found in the retroperitoneal space, and as a result, the doctor determined that there was no need to investigate the retroperitoneal space. Two factors have been highlighted that may have affected the surgical decisions at the time of treatment: (I) when the patient was sent to the hospital, the instrument that caused the injury during a violent attack was removed. The patient was not able to describe the instrument or the position in which he was injured because he was overly anxious and fearful. The patient was thin (175 cm, 65 kg), and his abdomen was flat. If information was available on the length of the instrument and the position of the patient when he was injured, the attending doctor could have decided to perform further examinations; (II) a CT scan was not available in the emergency operation room, and therefore, only B-mode ultrasound was performed before the surgery. The results suggested the possibility of hematomas in the retroperitoneal space adjacent to the upper pole of the right kidney. This information implied that the stab wound might have reached organs in the retroperitoneal space but was insufficient to confirm this. However, the attending doctor made the surgical decisions based upon what he/she observed during the operation. If the CT scan was available prior to the surgery, it may have helped to determine whether further investigations into the retroperitoneal space were necessary.
Second, there was doubt as to whether the clinical manifestations and the CT scan results suggested the risk of aortic rupture within four days after the exploratory laparotomy. After the surgery, the patient experienced abdominal pain that was not peritonitis, and it gradually eased and disappeared. It was difficult to determine if this intermittent, undefined abdominal pain was related to the aortic rupture. Due to the mixing of peritoneal fluid leakage with the remaining blood in the abdomino-pelvic cavity, the increase in abdominal hemorrhagic discharge following surgery did not necessarily indicate continued bleeding in the abdominal cavity. In addition, the discharge decreased over time, and the color turned lighter. The second exploratory laparotomy demonstrated that the massive hematoma caused by the aorta bleeding had formed only in the retroperitoneal space, and massive blood was not observed in the peritoneal cavity. After several red blood cell suspension transfusions, the patient’s Hgb level was low, and he was still slightly anemic, which can be explained by either (I) the blood volume increased after several transfusions were performed, and as a result, the Hgb level decreased or (II) a high energy-consumption state was caused by the stress response. Therefore, the low Hgb level was not definitive evidence of continued bleeding. A plain abdominal CT scan was conducted on the fourth day after the surgery and indicated that the retroperitoneal space adjacent to the middle part of the kidney was structurally vague. Several hematomas and a small amount of hemoperitoneum were found. A small amount of hemoperitoneum was also found in the perirenal space. This might have been a sign of aortic damage. However, due to the bleeding from the superior mesenteric vein and the fact that aortic rupture often causes massive bleeding, the attending doctor did not consider that an aortic rupture was possible, although it was not entirely ruled out. It would have been helpful if the enhanced CT scan could have been performed to provide potentially important information (3).
As for the possible pathophysiological process for delayed aortic rupture following perforating trauma, we speculated that when the patient was stabbed, the thick aorta wall was not cut through completely due to protection from multiple layers of tissues and organs. However, the sharp edge of the instrument had caused irreversible compression damage to the anterior and posterior walls of the aorta. Therefore, there was no tear or bleeding found in the aortic walls during the first exploratory laparotomy. Within five days following the surgery, with gradual tissue necrosis, the damaged aortic walls were eventually torn by the high-pressure aortic blood flow, and as a result, the patient died from the massive bleeding. Although pathophysiological evidence of this speculation is not available, discussion of the possible treatments is a valuable experience. Two situations could have occurred if the abdominal aorta was investigated during the first exploratory laparotomy: (I) the aortic rupture might have occurred in the damaged aortic wall after the retroperitoneal space was opened. It would have been difficult and highly risky to repair the rupture considering that the wound was adjacent to the renal arteries; (II) the aortic rupture might not have occurred in the damaged aortic wall after the retroperitoneal space was open. The damaged aortic wall might have been detected, and sutures could have been used to reinforce the damaged aortic wall. However, without opening the aorta, it would have been very difficult to determine if the posterior aortic wall directly behind the damaged anterior aortic wall was also damaged near the renal artery level. Under these circumstances, interventional treatment during or after the surgery would have been the best option (4-7). Stents placed in the potentially damaged parts of the abdominal aorta would have prevented the death resulting from a sudden aortic rupture following the posterior damage to the aortic wall. Additionally, the potential damages and risks associated with stent placement are lower than those of the vascular surgery.
This case demonstrated that it is very difficult to diagnose and treat a delayed aortic rupture following perforating trauma. Under similar circumstances in the future, if there is no evidence from the exploratory operation to suggest further investigation into the retroperitoneal space but aortic rupture can not be completely ruled out after reviewing the cause and depth of the injury, an enhanced CT scan is recommended to gain additional useful information. Even if the clinical manifestations and the results from the medical imaging report suggested a low possibility of aortic rupture, because of its high fatality rate, it is worth taking the risk and paying for an aortic angiogram and stent implantation.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Schumacher H, Böckler D, von Tengg-Kobligk H, et al. Acute traumatic aortic tear: open versus stent-graft repair. Semin Vasc Surg 2006;19:48-59. [PubMed]
- Cherry JK, Bennett DE. False aneurysm of the aorta following penetrating trauma. Report of a case with secondary infection and delayed rupture. Arch Surg 1966;93:404-8. [PubMed]
- Rakita D, Newatia A, Hines JJ, et al. Spectrum of CT findings in rupture and impending rupture of abdominal aortic aneurysms. Radiographics 2007;27:497-507. [PubMed]
- Canaud L, Alric P, Branchereau P, et al. Open versus endovascular repair for patients with acute traumatic rupture of the thoracic aorta. J Thorac Cardiovasc Surg 2011;142:1032-7. [PubMed]
- Geisbüsch P, Leszczynsky M, Kotelis D, et al. Open versus endovascular repair of acute aortic transections--a non-randomized single-center analysis. Langenbecks Arch Surg 2009;394:1101-7. [PubMed]
- Stone DH, Brewster DC, Kwolek CJ, et al. Stent-graft versus open-surgical repair of the thoracic aorta: mid-term results. J Vasc Surg 2006;44:1188-97. [PubMed]
- Amabile P, Collart F, Gariboldi V, et al. Surgical versus endovascular treatment of traumatic thoracic aortic rupture. J Vasc Surg 2004;40:873-9. [PubMed]


